Use visual tools to explain this treatment option to patients
The COVID-19 pandemic has had a negative impact on our eyes. Dry eye disease (DED) symptoms have risen, largely due to the increased use of screens as more of us are working and learning remotely, as well as the wearing of face masks. Ill-fitting masks can expose the eyes to a constant flow of exhaled air, causing a rapid evaporation of tears.
So it was ideal that this summer the iTear100 (Olympic Ophthalmics) was approved by the FDA. The timing was especially good because Allergan’s TrueTear neurostimulation device for the treatment of DED was discontinued. Patients who had success with TrueTear would have had no replacement option. But now, patients have access to the iTear100, an easier approach to neurostimulation to produce tears. The device alone isn’t enough to ensure patient understanding and adherence, however. That’s where an interactive anatomy tool like Rendia’s Exam Mode comes in.
A new, external neurostimulation device
Unlike TrueTear, which was an intranasal device that delivered small electrical currents to sensory neurons of the nasal cavity, the iTear100 is an electromechanical nerve stimulator applied externally to the soft nasal fold of the nose. Like TrueTear, it also requires a prescription by an eye care provider. Patients apply the handheld, noninvasive device to the outside of the nose for up to 30 seconds per side to activate the trigeminal parasympathetic pathway via a sonic frequency. It can be used as needed throughout the day, for up to 30 days at a time.
The iTear100, available by prescription, is an electromechanical nerve stimulator applied externally to the soft nasal fold of the nose.
After one month the iTear100 device requires reactivation. Currently, the patient can exchange the device through the company or their doctor’s office. In the near future, the patient will receive a reactivation code electronically or via an app, at the discretion of the eye care practitioner.
In clinical studies, Schirmer’s scores, fluorescein staining, tear break-up time, and meibomian gland scores all improved statistically and immediately. These results were maintained over the intermediate and long term (180 days). Furthermore, Ocular Surface Disease Index scores showed statistical improvement at every study visit. Safety and patient comfort scores showed a favorable risk-benefit ratio with only 3 percent of the study population reporting adverse events which included sneezing, tickling or headaches, and 1 percent noted nasal pain.
A better alternative to artificial tears
The iTear100 technology is an exciting new option to add to your armamentarium, because our natural tear secretion is far more complex and potent than artificial tears, containing nerve growth factors and thousands of mucins, proteins and lipids. Research shows that neurostimulation affects more than reflex tearing as meibomian gland secretion, mucin and aqueous tears have all been shown to be produced via neurostimulation. Patients in the study who stated they frequently rely on artificial tears were able to decrease artificial tear use (44.2% of patients) or eliminate them altogether (23.4%).
Studies show that patients using neurostimulation were able to decrease or eliminate their use of artificial tears.
It is easy to prescribe and get patients started on this new treatment, as it fits really well into the current telehealth environment. Basically, a doctor can go to the www.myitear.com website, sign up, receive training, and prescribe the treatment in about 10 minutes. Similarly, the patient can go to the same website and sign up and as long as they have a prescription on file, and the company will send them a device.
It’s good to see a new neurostimulation device on the market, as many dry eye patients who had success with TrueTear are looking for an alternative. The external application of the iTear100 makes it an easy treatment option for doctors, staff and patients.
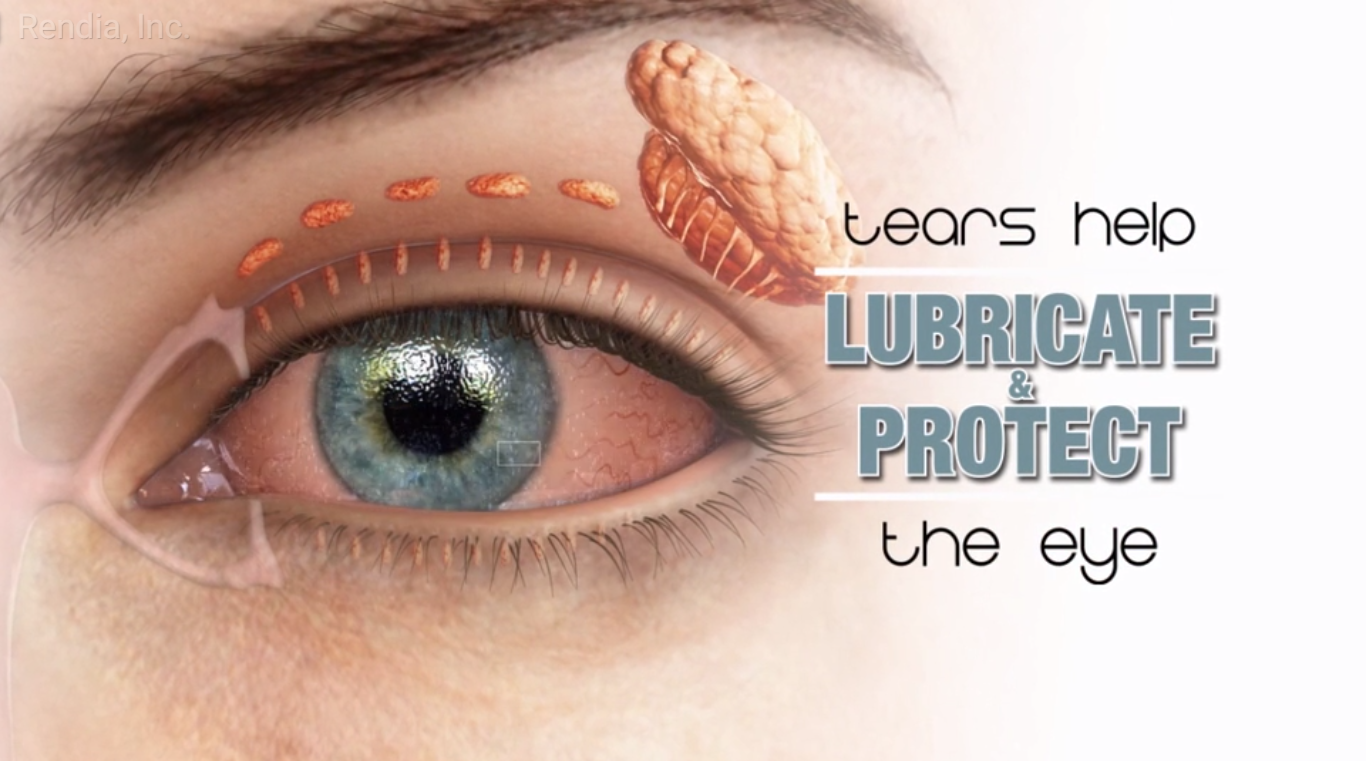
When it comes to explaining dry eye disease to patients, I find it most effective to use visual aids to accompany the discussion. I explain that while the symptoms include dryness, redness, or blurry vision, the anatomical causes of DED can be complex. I use Exam Mode to illustrate meibomian gland dysfunction and poor tear quality.
Watch my 5-minute demonstration video here.
The views expressed above are of Dr. Paul Karpecki and do not necessarily represent those of Rendia.