Why eye doctors are better suited than other providers to treat conjunctivitis
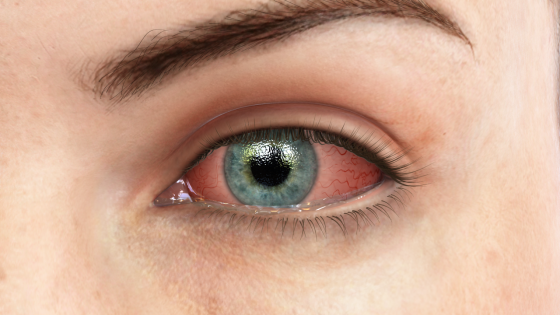
Many parents know that telltale itchiness, “goopiness,” and redness of their child’s eyes probably mean one thing: pink eye. Acute conjunctivitis is a common problem, affecting an estimated 6 million people each year in the U.S. But what many parents don’t know is that they shouldn’t automatically take a child with pink eye to the pediatrician. Here’s what to let your patients, and parents of patients, know about this eye condition.
The three types of conjunctivitis
Many people do not know that there are three main types of conjunctivitis: viral, bacterial, and allergic. You might share with your patients this information from the National Eye Institute:
1. Viral conjunctivitis is commonly caused by adenovirus and herpesvirus, and may also occur along with an upper respiratory tract infection, cold, or sore throat.
2. Bacterial conjunctivitis is caused by infection of the eye with bacteria such as Staphylococcus aureus, Streptococcus pneumonia, or Haemophilus. Because it is highly contagious, it is a common reason for children to stay home sick from day care or school.
3. Allergic conjunctivitis can be caused by allergies to pollen, dust mites, molds, or animal dander.
Eye doctors know it can be hard to distinguish between viral and bacterial conjunctivitis simply by looking at a patient.
Of course, as eye doctors know, it can be hard to distinguish between viral and bacterial conjunctivitis simply by looking at it. And anyway, most patients will be more concerned with how to treat the pink eye than what caused it.
The danger of overprescribing antibiotics
Many doctors prescribe anyone presenting with pink eye symptoms with a topical antibiotic in case it is bacterial, noted Mallika Marshall, M.D., on the Harvard Health Blog. “However, according to ophthalmologists bacterial conjunctivitis often goes away on its own, and the practice of treating everyone ‘just in case’ is irresponsible.”
A new study shows that most acute conjunctivitis patients get the wrong treatment; about 20 percent receive an antibiotic that can worsen the infection.
She cites a new study published in the journal Ophthalmology that suggests that most people with acute conjunctivitis are getting the wrong treatment. About 60 percent of patients are prescribed antibiotic eye drops, even though antibiotics are rarely necessary to treat this common eye infection. About 20 percent receive an antibiotic-steroid eye drop that actually can prolong or worsen the infection.
The study also found that primary care providers (family physicians, pediatricians, internal medicine physicians, and urgent care providers) diagnose a majority (83 percent) of conjunctivitis patients. Only a minority were diagnosed by eye care providers such as ophthalmologists or optometrists. And yet patients diagnosed by a primary care provider were two to three times more likely to fill prescriptions for antibiotic eye drops than patients diagnosed by an ophthalmologist.
How to help patients instead
As the American Academy of Ophthalmology (AAO) noted, “Antibiotics are rarely necessary to treat acute conjunctivitis. Most cases are caused by viral infections or allergies and do not respond to antibiotics. Antibiotics are often unnecessary for bacterial conjunctivitis because most cases are mild and would resolve on their own within 7 to 14 days without treatment.”
Eye doctors can teach patients simple ways to ease pink eye symptoms, such as warm or cool compresses, artificial tears, and antihistamines.
Teach patients that there are some simple things they can do to ease pink eye symptoms, suggested Dr. Marshall: “Warm compresses can help loosen eyelid crusting. Cool compresses and artificial tears can soothe irritated eyes. Over-the-counter eye drops and antihistamines can help ease the itching and tearing associated with allergic conjunctivitis.”
Your message to patients should be: if you think you or your child has conjunctivitis, call your eye doctor. And don’t get upset if the doctor does not prescribe antibiotics. Said Dr. Marshall: “They are doing you and the public at large a favor.”
For more information on patient education for your eye care practice, and for a free trial of Rendia, get in touch with us today!