Sufferers have increased and adherence has dropped during the pandemic; why patient education is key
A year ago, the Ophthalmology Times reported on the prevalence of dry eye disease (DED), calling it a “critical and significant public health issue” in the U.S. While a 2017 study estimated that 16 million Americans have been diagnosed with DED, the actual number of people suffering from dry eye is likely much higher—with some reports indicating that nearly half of all U.S. adults experience dry eye signs and symptoms.
And that was before the global coronavirus pandemic. Since COVID-19 began shutting down schools, workplaces, and businesses in the U.S. in March, people have been spending more time indoors, more time on screens, and more time wearing facemasks. These are all factors that have the potential to create or worsen dry eye symptoms. Find out what you can do for new and existing DED patients now, both virtually and in your office.
Eye problems increasing during the pandemic
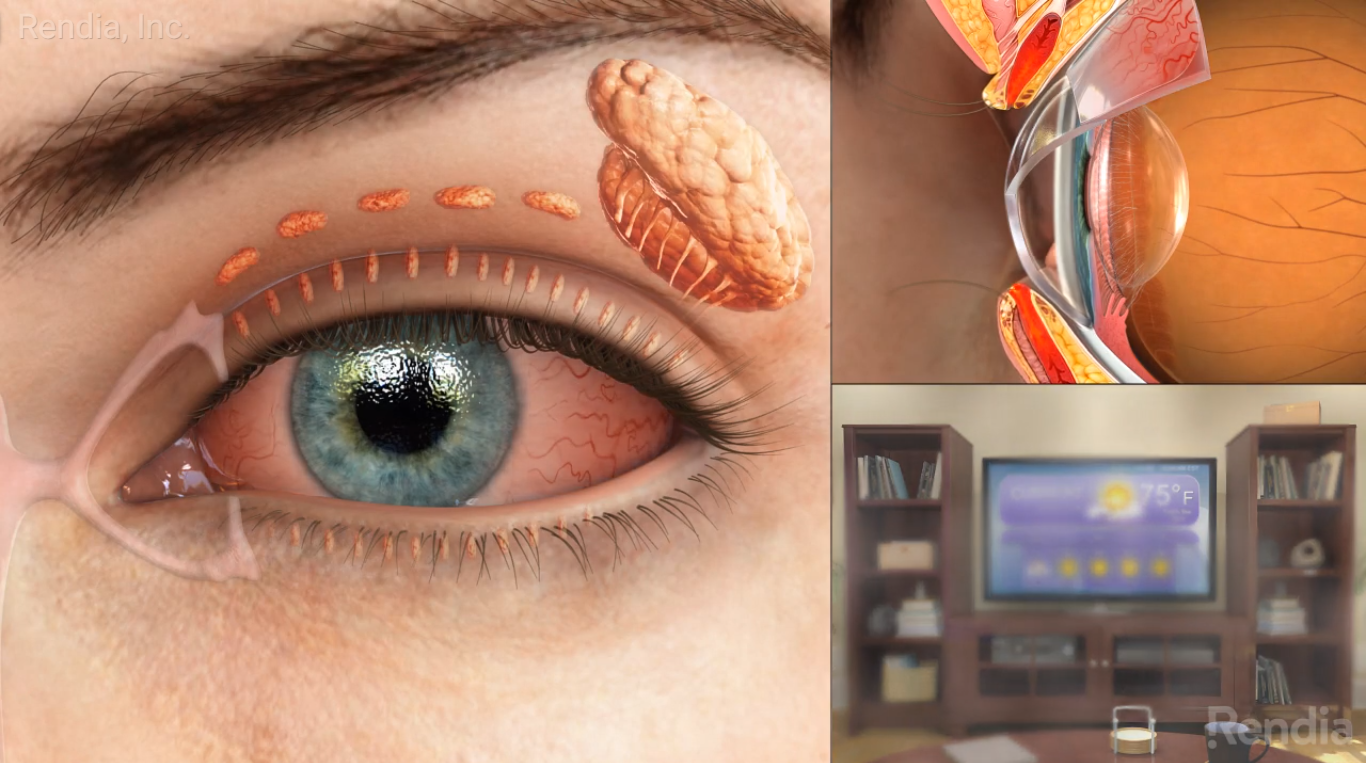
As eye doctors know, symptoms of dry eye may include watery eyes, a burning or gritty sensation in the eyes, blurred vision, and sensitivity to light. But many of the millions of people who are now working from home and spending all day on computers might not make the connection between their change in work environment and their ocular symptoms.
“It is not surprising to see increases in symptomatic complaints of burning, watering, ocular pain, eye strain, and intermittent blur,” wrote Jade Coats, O.D., in an Optometry Times article titled, “5 common ocular problems seen during the pandemic.” Computer-induced dry eye is number one.
Increased use of computers and digital devices, along with stress and anxiety, can explain why ocular problems including dry eye are on the rise during COVID-19.
Explain to patients that we tend to blink less often when using computers or digital devices, which can cause eye dryness and irritation. Let them know that digital eye strain, also called Computer Vision Syndrome (CVS), can also be caused by such factors as poor lighting, screen glare and uncorrected vision problems. Be sure to ask your patients about their home office or workstation setup. Show them this video for eye-friendly exercises they can do throughout the day:
How masks can exacerbate symptoms
The second most common problem Dr. Coats is seeing in her patients during the pandemic is mask-induced dry eye. This is “likely due to the constant flow of exhaled air on the exposed eye while breathing. Sometimes presenting with ocular pain and intrapalpebral corneal staining, the escaping air flow can create a windy obstacle affecting tear film stability,” she wrote. There seems to be a correlation with the frequency of mask wearing—for instance, in healthcare workers who wear masks for 40+ hours a week—and it is “especially worsened with ill-fitting masks.”
Wearing facemasks for long periods of time, especially ill-fitting masks, can expose the eyes to a constant flow of air, worsening dry eye symptoms.
Dr. Coats advises providers to ask questions about mask usage when evaluating a patient’s overall risk factors for DED, and to educate patients on the importance of a properly fitting mask to reduce airflow directed at the eyes.
For more on how to help your patients now, read Masks and Foggy Glasses: Caring for Your Optical Patients.
Why some patients are struggling with adherence
In addition to diagnosing new cases of DED, some eye doctors are finding that symptoms are worse in their existing dry eye patients who have already been prescribed treatments. What’s the explanation? Cynthia Matossian, M.D., discovered it was a compliance problem.
During telemedicine visits, she became aware that many of her patients were not keeping up with their treatment regimens. For some, this was because they didn’t understand the reasons behind what was prescribed, noted Dr. Matossian in the Ophthalmology Times. For instance, one patient mistakenly thought that one thermal pulsation treatment would fix her problems forever, saying, “My glands have been ‘cleaned out’ now, right?” Dr. Matossian wrote, “We talked about how she sees her dental hygienist twice a year, and that, in a similar fashion, we have to continue to maintain lid and meibomian gland health over time.”
A misunderstanding of prescribed treatments as well as a disruption to their regular routines can lead to nonadherence for many dry eye patients.
For other patients, noncompliance is due to such factors as the disruption to their routines, the demands of homeschooling, and additional stress in general. Dr. Matossian discovered that some patients were taking their omega-3 fatty acid supplements erratically or using their eye drops on an as-needed basis rather than twice daily as prescribed.
In all cases, patient education is the answer. People only absorb a fraction of what their doctors say during an in-person office exam or telemedicine visit, wrote Dr. Matossian, “so I’m realizing that we need to give instructions in many different formats.” Send patients this video before the appointment, then use Exam Mode during your virtual exam to help them understand the anatomy of dry eye. Sending them this video afterwards to encourage adherence, and this video to touch base with patients you haven’t seen in awhile, who may not realize their symptoms are related to dry eye.
In-office procedures may be the answer
Many of Dr. Matossian’s dry eye patients admitted they could not adhere to a consistent at-home treatment regimen right now. “Either they were generally not good at remembering to use drops twice a day or their drop instillation was tied to a routine that was now gone. That’s where procedures come in.” Educate patients on why they may experience relief from dry eye symptoms with an in-office meibomian gland procedure.
The pandemic has presented numerous challenges for both dry eye sufferers and the providers who treat them. Eye doctors must figure out how to help patients remotely, while also encouraging them to safely return to their offices for recommended procedures if necessary. Proactive outreach and ongoing patient education is a smart approach to reaching the growing number of dry eye sufferers in the U.S.
Addressing the needs of dry eye patients is a great way to attract loyal patients who have been overlooked or misdiagnosed. It’s a smart business strategy, too. Download our eBook to find out how to build a Dry Eye Center of Excellence in your practice.